Improved Cookstoves Halve Air Pollution Peaks, But Ambient Exposure Dampens Health Benefits

Improved cookstoves can cost-effectively reduce emissions, save households up to $85 per year in charcoal expenditures, and reduce peak cooking emissions by 40%. However, this has limited health impacts in contexts with high ambient pollution.
At a Glance
Key Challenge
Billions of urban poor face both high ambient air pollution concentrations, often caused by industrial emissions, and even higher transient peaks, often caused by private activities such as cooking.
Policy Insight
Ambient air pollution dampens the health benefits of improved cookstoves. Chronic health improvements will likely require addressing negative externalities through environmental regulation.
The adoption of an improved cookstove in Nairobi, Kenya can reduce carbon dioxide (CO2) emissions by 3.5 tons per year (Berkouwer and Dean, 2022). Factoring in the additionality rates, cookstove subsidies (financed, for example, through carbon credits) would reduce emissions at a cost of less than $5 per total carbon dioxide content (tCO2)-equivalent, which is much more cost-effective than most available abatement alternatives. In addition, improved stoves can save households up to $120 per year in charcoal expenditures. But what are the effects of the adoption of a modern stove on air pollution and health in the long term?
According to the World Health Organization (WHO), air pollution is “the single biggest environmental threat to human health” (WHO 2017). It is responsible for 7-9 million premature deaths annually, or 10-15% of all deaths. More than 90% of those deaths occur in low- and middle-income countries (LMICs) (Lancet 2017).
Air pollution can be broadly categorized into two distinct categories: household-generated air pollution (HAP) and ambient air pollution (AAP). HAP is generated by household activities such as cooking—according to the World Bank (2020b), “4 billion people are without access to modern energy cooking services”. AAP is generated by other people or businesses, for example through transportation, energy generation, industrial activity, waste disposal, or other economic activity.
The 2 billion people who live in cities in LMICs are uniquely exposed to both high average AAP as well as even higher transient peaks in HAP. For them, adopting cleaner cooking technologies may reduce their HAP, but because of their continued exposure to high levels of AAP generated by other sources of air pollution this may or may not improve their health. In this type of context, how much do clean cooking technologies improve health?
This question is difficult to answer, and answering it well requires several key ingredients:
- It is not sufficient to look at correlations between pollution and health. Since higher-income families tend to live in urban neighborhoods with cleaner air, correlations between pollution and health could be driven by lower-income families’ lack of access to nutrition or health care. However, a recent review in the Lancet Global Health found that only 6 of 437 papers studying pollution and health were randomized trials (Lee et al. 2020).
- Health benefits may compound over years, but following up with households several years after cookstove adoption can be difficult logistically. Urban households frequently move around, and households may also change cooking technologies between the initial adoption and the long-term follow-up survey.
- Air pollution can vary minute-to-minute depending on what activity someone is engaged in (say, cooking, sleeping, working, or commuting) and whether they are indoors or outdoors. Measuring an individual’s true air pollution exposure accurately thus requires using personal monitors that are co-located with the individual, and which take high-frequency pollution recordings.
Our recent working paper, “Private actions in the presence of externalities: The health impacts of reducing air pollution peaks but not ambient exposure,” tackles this question (Berkouwer and Dean, 2023). In a previous study, we provided 1,000 households in Nairobi, Kenya with the opportunity to adopt an improved charcoal cookstove. We found that improved stoves could reduce charcoal usage by 39% (saving households more than $100 per year in charcoal expenditures, with an investment return of 300% on the $40 cost of the stove) and that access to credit was a key driver of adoption (Berkouwer and Dean, 2022). The current study followed up with these households three years later to measure the long-term impacts of improved stove adoption on pollution exposure and health.
Improved Cookstove Adoption Among the Urban Poor
Three billion people are expected to live in slums in Africa and Asia by 2050 (UN, 2022). Across many cities in Sub-Saharan Africa, more than 80% of residents use biomass as their primary cooking energy (FAO, 2017). Charcoal usage is expected to continue growing in coming decades due to rising incomes and rapid urbanization, as households that currently gather firewood for cooking adopt charcoal cooking technologies (Hanna and Oliva, 2015).
However, most of the existing literature studying the health impacts of improved cookstove adoption focuses on rural populations. This includes, for example, the RESPIRE trial in rural Guatemala (McCracken et al., 2007; Smith et al., 2011; Smith-Sivertsen et al.; 2009) and the more recent HAPIN trial in Guatemala, India, Peru, and Rwanda (Clasen et al. 2022). One notable exception is Alexander et al (2018), which studies the impact of ethanol cookstove adoption by pregnant women on birthweight and other pregnancy outcomes in Ibadan, Nigeria.
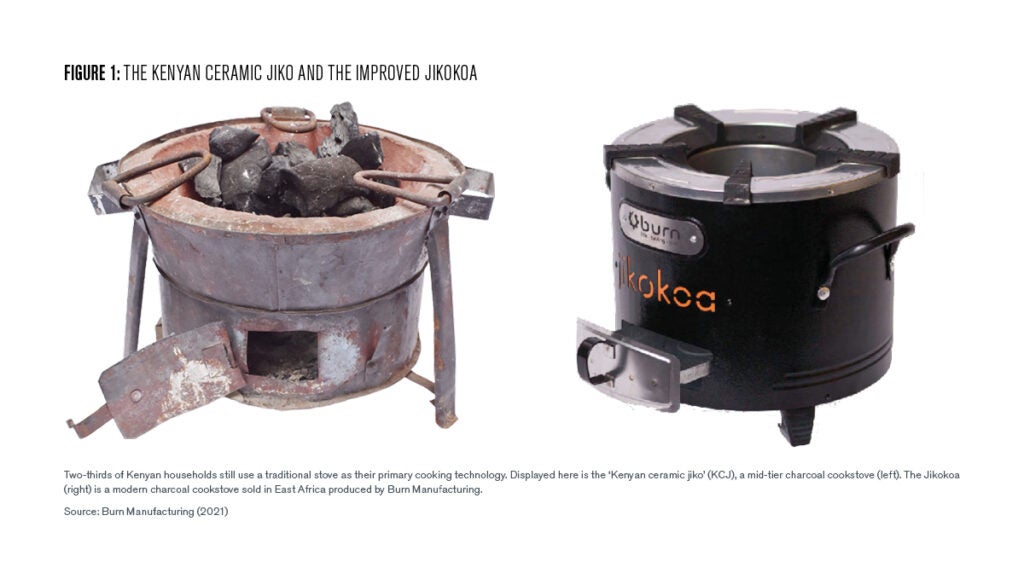
To answer our research question, our study enrolled 1,000 households residing in informal settlement areas around Nairobi. Within each household, we surveyed the primary cookstove user—95% of whom were women—and also asked questions about the health of any children under five years old who spent significant amounts of time in the home. At baseline, all households were using a Kenyan Ceramic Jiko (KCJ), shown on the left in Figure [1]. In Kenya, more than two-thirds of households still use a KCJ or other traditional wood and charcoal stoves as their primary cooking technology (Kenya 2019 Census).
The Improved Jikokoa Cookstove
We studied the Jikokoa, an improved charcoal cookstove produced by Burn Manufacturing, available for around $30 in stores and supermarkets across Africa (shown on the right in Figure 1). The cooking experience of using the Jikokoa is very similar to the KCJ: respondents report no change in the taste or smell of food, they can continue buying the same charcoal from their preferred vendor, and effectively no learning is required to switch from the KCJ to the Jikokoa. In 2019, different study participants received different subsidies for the Jikokoa, causing some study participants to adopt the stove and others to continue using the KCJ (Berkouwer and Dean, 2022). By comparing improved stove users and KCJ users, this allowed us to study the long-term impacts of improved stove ownership.
A key concern when conducting a long-term follow-up survey is whether study participants still own the cookstoves they originally adopted. Reassuringly, this was the case. Three years after the initial surveys, 83% of respondents who purchased a Jikokoa still owned one, and 90% of respondents who did not purchase a Jikokoa still did not own one. Reflecting widespread adoption of liquid petroleum gas (LPG) cookstoves globally, around 50% of respondents owned an LPG stove (and this is balanced across those who adopted the Jikokoa and those who didn’t), up from around 20% in 2019, possibly due to ongoing government LPG subsidies. Fuel stacking is thus common: respondents who own both a charcoal stove and an LPG stove often report using their LPG stove when wanting to cook a quick, small meal or a hot drink and using their charcoal cookstove for larger daily meals such as maize or beans.
To measure air pollution as directly experienced by cookstove users, study participants received personally wearable monitors that record high-frequency air pollution measurements. The implementation of this deployment benefited from a close collaboration with the Berkeley Air Monitoring Group, who have extensive experience conducting similar research (see, for example, Chillrud et al. 2021; Gould et al. 2022; Johnson 2021; Burrowes et al. 2020).
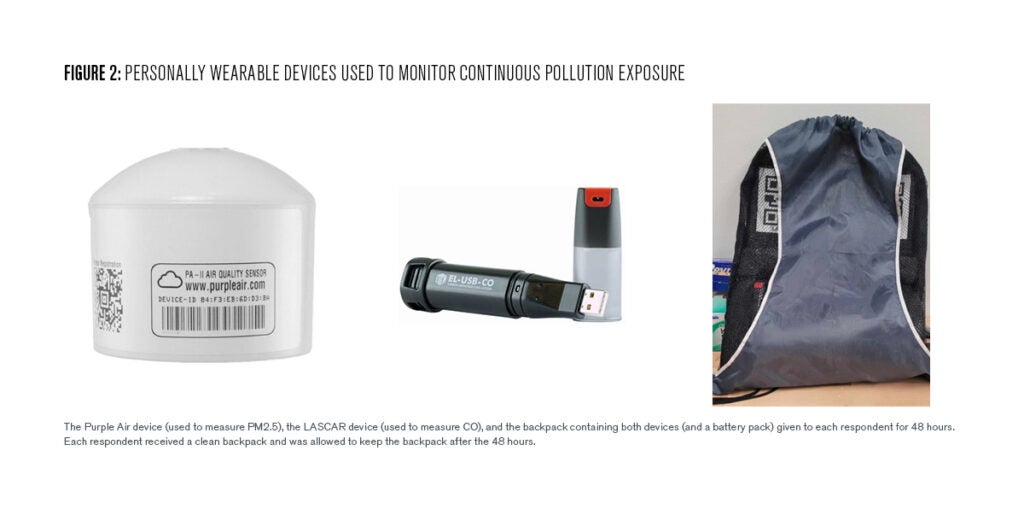
Each respondent was asked (and compensated) to wear a backpack containing two air pollution monitoring devices and a battery pack. The Purple Air device recorded particulate matter below 1.0 or 2.5μm in diameter (PM1.0 and PM2.5, respectively, measured in ug/m3) once every two minutes. The LASCAR device recorded parts-per-million of carbon monoxide (CO, measured in ppm) once every minute. Respondents kept the backpacks for 48 hours, during which the devices were continuously measuring air pollution. The purple air device, the LASCAR device, and the backpack containing both devices (together with a battery pack) are shown in Figure [2]. We recorded data between October and April, and we saw no seasonal differences over this period.
To determine which health outcomes to focus on, and to develop rigorous survey procedures to measure these in the field, we spoke with numerous public health researchers and consulted the existing public health literature related to cookstoves. To get a comprehensive picture of respondent health, we conducted a wide range of quantitative and self-reported measures of health. Quantitatively, enumerators measure respondents’ blood oxygen levels and blood pressure, following the standard methodology prescribed by Centers for Disease Control and Prevention National Health and Nutrition Examination Survey (CDC NHANES, 2019).
Enumerators also collected child development outcomes such as height, weight, and arm circumference. They also asked about 13 different self-reported health diagnoses by a health professional (such as pneumonia, asthma, and cardiovascular disease) as well as 26 self-reported health symptoms that include respiratory symptoms (such as a runny nose, persistent cough, sore throat, breathlessness, or wheezing) as well as non-respiratory symptoms (such as skin rash, weight loss, or chronic tiredness).
To measure cognitive well-being, enumerators conducted the Reverse Corsi Block task to measure working memory (Brunetti et al. 2014), the Hearts and Flowers task to measure response inhibition (Davidson et al., 2006), and the d2 task to measure sustained attention (Bates and Lemay Jr. 2004; Brickenkamp and Zillmer 1998). Finally, we asked about health behaviors such as doctor visits and health expenditures.
The Charcoal and Pollution Impact of Improved Cookstoves
Our first finding is that the financial savings identified in Berkouwer and Dean (2022), conducted among a sample of households residing in Nairobi, largely persist: even three years after adoption, stove ownership causes charcoal expenditures to decrease by 39%. Ninety-two percent of respondents continue to live in Nairobi, where households often spend up to 10-20% of income on energy expenditures. For these households, the financial savings from reduced charcoal expenditures add up to around USD 1.65 per week (those who continue to use a traditional stove as their primary cookstove spend around USD 3.80 per week).
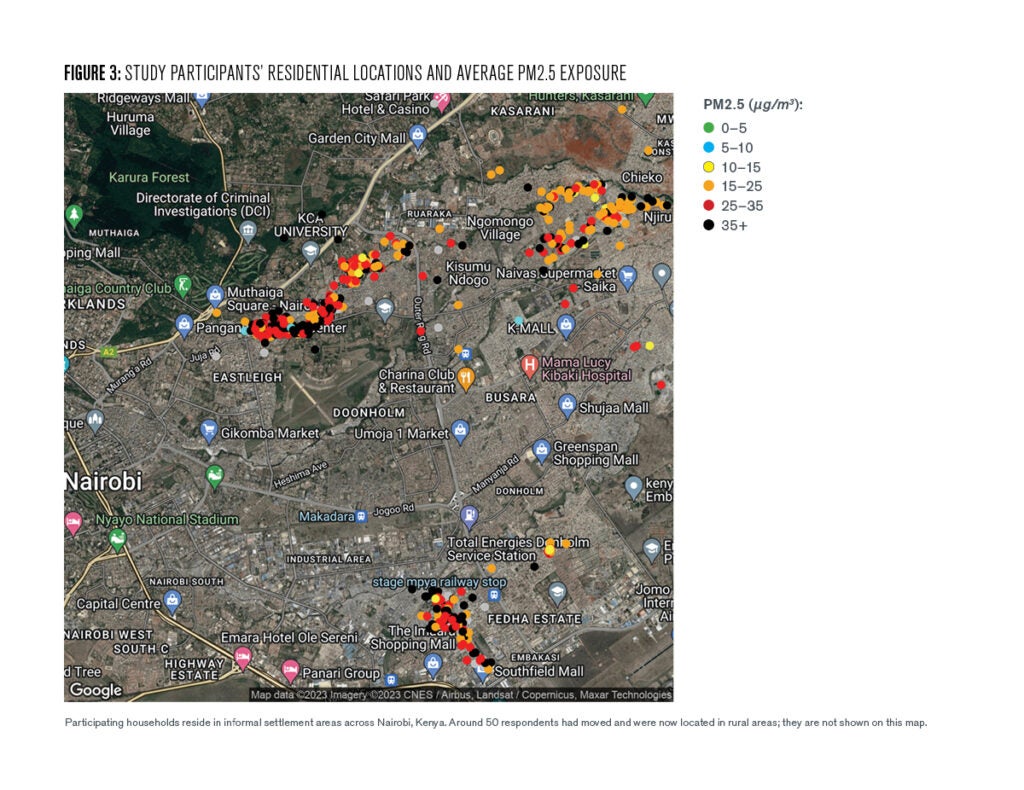
Turning to the PM2.5 air pollution data, we find that most respondents experience air pollution levels well in excess of the WHO’s recommended standard of 5 ug/m3 on a daily basis. Figure [3] shows the residential locations of study participants across Nairobi, as well as their average pollution exposure (in PM2.5) over the approximately 48 hours during which they were wearing the pollution monitors.
The data indicate that the impact of improved cookstove adoption on air pollution exposure is complex. We use the self-reported time use data to determine during which of the 48 hours each respondent is cooking. To begin, the average level of median non-cooking pollution is 25 ug/m3. For many respondents the worst 15 minutes of air pollution experienced each day occurs during cooking. For participants cooking with their old charcoal cookstove, the worst 15 minutes of air pollution experienced during cooking is, on average, 150 ug/m3—a 125 ug/m3 increase.
However, adoption of the improved Jikokoa stove decreases this by 52 ug/m3, or around 42%. This number coincides exactly with the reduction in charcoal expenditures caused by improved cookstove adoption and is therefore likely a direct result of needing less charcoal to cook the same meals. Figure [4] below shows the hourly differences graphically: average hourly pollution is similar for users of the improved stove and the traditional stove during most hours of the day but is lower for improved stove users during key cooking hours.
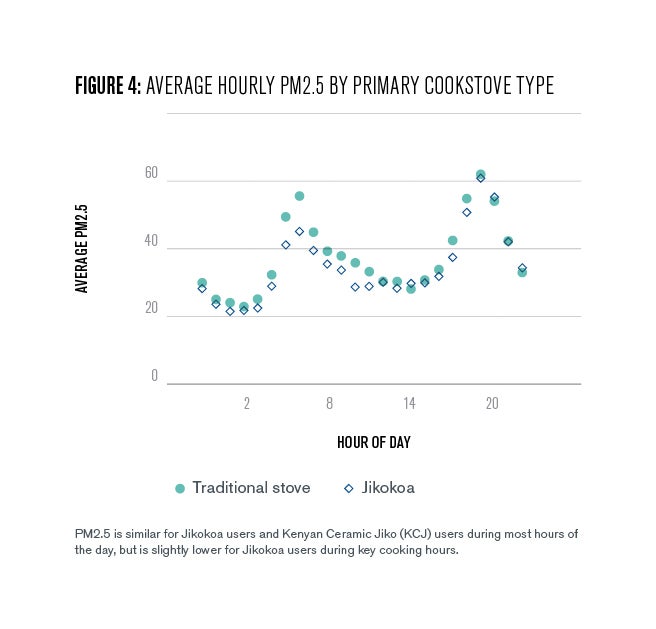
Adoption of the improved stove also causes a modest reduction in time spent cooking each day, likely because the stove lights and heats up more quickly than their old charcoal stoves. As a result, average pollution during the most polluted cooking hour is 67 ug/m3 higher than ambient levels, but adoption of the improved Jikokoa stove reduces this increase by 31 ug/m3, or around 46%.
While the reduction in air pollution during cooking is very large, households only cook for two hours per day on average. Adoption of the improved stove does not cause any changes in ambient pollution—generated, for example, by traffic, nearby factories, or industrial machinery—during the remaining 22 hours of the day. Given the high levels of pollution during these other hours, the effect of improved stove adoption on average daily PM2.5 exposure is very small and not statistically different from zero.
We find no impacts on carbon monoxide. This is in line with recent laboratory tests performed by the Centre for Research in Energy and Energy Conservation (CREEC) at Makerere University in Uganda. CREEC scored the Jikokoa G3.5 as Tier 3 for PM2.5 but Tier 1 for CO (a more recent version of the Jikokoa achieves Tier 2 for CO), resulting from a desire to increase the durability and efficiency of the stove by limiting peak cooking temperatures to 700◦C. While this improves durability and efficiency of the stove, it limits oxygenation and increases the production of CO instead of CO2 while cooking.
The Health Benefits of Reduced Pollution Spikes
The improved stove reduced pollution spiked during hours when study participants were cooking but did not meaningfully reduce average aggregate daily PM2.5 exposure. How does this combination affect cookstove users’ health?
Our first key result is that the improvement in pollution during cooking spikes causes a 28% reduction in the number of respiratory health symptoms that respondents report (0.24 standard deviations). This is driven by reductions in the fraction of people who self-report having had a sore throat, headache, persistent cough, or tiredness in the past month.
Short spikes in pollution may therefore be responsible for these types of health symptoms. This is confirmed when we investigate the relationship between pollution exposure and health symptoms in a separate regression: the maximum of hourly average pollution is correlated with self-reported health symptoms, whereas average pollution and the duration of high pollution exposure are not.
However, despite these improvements in self-reported health, we find no meaningful improvements in blood pressure, blood oxygen, self-reported non-respiratory symptoms, or self-reported diagnoses as made by health professionals. It may be that these health symptoms only improve with prolonged reductions in average levels of pollution exposure beyond the three years that we observe.
One concern with relying on the self-reported health symptoms is that they may be inaccurate, for example because respondents who received a sizeable subsidy to adopt an improved stove may feel some pressure to self-report health improvements to the surveying team. However, additional data tests suggest that the effects above are likely strongly driven by real health outcomes. First, conditional on adopting the improved stove, we do not see that respondents who received larger subsidies report fewer symptoms than respondents who received only a small subsidy. Second, even controlling for subsidy size, we see a strong correlation between pollution and self-reported health symptoms.
Policy Implications of Improved Cookstoves
These findings have important policy implications. On the one hand, households can meaningfully reduce short-term health symptoms themselves, by adopting improved cooking technologies that reduce air pollution peaks during cooking.
On the other hand, households who live in urban areas with high ambient pollution concentrations may see little change in average pollution exposure from adopting an improved cookstove. Significant improvements to chronic underlying health conditions—such as blood pressure, blood oxygen, and pneumonia—may only be achieved by reducing average levels of pollution, which urban households themselves have little control over. These types of longer-term benefits will require government intervention regulating the negative externalities generated by transportation and industrial activity.
This study has human subjects research approval in Kenya (KEMRI/RES/7/3/1 and AMREF ESRC P1195/2022) and the US (University of Chicago IRB22-0943 and Penn IRB# 849048). This academic research was conducted independently and Burn Manufacturing has provided no funding for this research. Read the disclosure statement.
Susanna Berkouwer
Assistant Professor of Business Economics & Public PolicySusanna Berkouwer is an assistant professor of Business Economics & Public Policy at the Wharton School.
Joshua Dean
Assistant Professor, University of ChicagoJoshua Dean is an assistant professor of behavioral science and economics at the University of Chicago Booth School of Business.
Alexander, D. A., Northcross, A., Karrison, T., Morhasson-Bello, O., Wilson, N., Atalabi, O. M., Dutta, A., Adu, D., Ibigbami, T., Olamijulo, J., Adepoju, D., Ojengbede, O., & Olopade, C. O. (2018). Pregnancy outcomes and ethanol cook stove intervention: A randomized controlled trial in Ibadan, Nigeria. Environment International, 111, 152–163.
Bailis, Robert, Rudi Drigo, Adrian Ghilardi, and Omar Masera. 2015. “The Carbon Footprint of Traditional Woodfuels.” Nature Climate Change 5:266–272.
Bates, M. E., & Lemay Jr., E. P. (2004). The d2 Test of Attention: Construct Validity and Extensions in Scoring Techniques. Journal of the International Neuropsychological Society, 10, 392–400.
Berkouwer, S. B., & Dean, J. T. (2022). Credit, attention, and externalities in the adoption of energy efficient technologies by low-income households. American Economic Review, 112 (10).
Berkouwer, S. B., & Dean, J. T. (2023). Pollution exposure and health: The role of private actions and environmental externalities in Nairobi. National Bureau of Economic Research Working Paper #31614. Available here: https://sberkouwer.github.io/BerkouwerDean_Health.pdf.
Brickenkamp, R., & Zillmer, E. (1998). The d2 Test of Attention. Hogrefe & Huber.
Brunetti, R., Del Gatto, C., & Delogu, F. (2014). eCorsi: Implementation and Testing of the Corsi Block-tapping Task for Digital Tablets. Frontiers in Psychology, 5, 1–8.
Burrowes, V. J., Piedrahita, R., Pillarisetti, A., Underhill, L. J., Fandino-Del-Rio, M., Johnson, M., Kephart, J. L., Hartinger, S. M., Steenland, K., Naeher, L., Kearns, K., Peel, J. L., Clark, M. L., Checkley, W., & HAPIN Investigators. (2020). Comparison of next-generation portable pollution monitors to measure exposure to PM2.5 from household air pollution in Puno, Peru. Indoor Air, 30 (3), 445–458.
Centers for Disease Control and Prevention. (2019). National Health and Nutrition Examination Survey: Blood Pressure Procedures Manual (CDC HANES).
Chillrud, S. N., Ae-Ngibise, K. A., Gould, C. F., Owusu-Agyei, S., Mujtaba, M., Manu, G., Burkart, K., Kinney, P. L., Quinn, A., Jack, D. W., & Asante, K. P. (2021). The effect of clean cooking interventions on mother and child personal exposure to air pollution: Results from the Ghana randomized air pollution and health study (GRAPHS). Journal of Exposure Science & Environmental Epidemiology, 31 (4), 683–698.
Clasen, T. F., H. H. Chang, L. M. Thompson, M. A. Kirby, K. Balakrishnan, et al. (2022). Liquefied Petroleum Gas or Biomass for Cooking and Effects on Birth Weight. New England Journal of Medicine, 387:1735-1746.
Davidson, M. C., Amso, D., Anderson, L. C., & Diamond, A. (2006). Development of Cognitive Control and Executive Functions from 4 to 13 Years: Evidence from Manipulations of Memory, Inhibition and Task Switching. Neuropsychologia, 44 (11), 2037–2078.
Food and Agricultural Organization of the United Nations. 2017. The Charcoal Transition.
Gould, C. F., Mujtaba, M. N., Yang, Q., Boamah-Kaali, E., Quinn, A. K., Manu, G., Lee, A. G., Ae-Ngibise, K. A., Carrión, D., Kaali, S., Kinney, P. L., Jack, D. W., Chillrud, S. N., & Asante, K. P. (2022). Using time-resolved monitor wearing data to study the effect of clean cooking interventions on personal air pollution exposures. Journal of Exposure Science & Environmental Epidemiology.
Hanna, Rema, Esther Duflo, and Michael Greenstone. 2016. “Up in Smoke: The Influence of Household Behavior on the Long-Run Impact of Improved Cooking Stoves.” American Economic Journal: Economic Policy 8 (1): 80–114.
Hanna, Rema, and Paulina Oliva. 2015. “Moving Up the Energy Ladder: The Effect of an Increase in Economic Well-Being on the Fuel Consumption Choices of the Poor in India.” American Economic Review Papers and Proceedings 105 (5): 242–246.
Iiyama, Miyuki, Audrey Chenevoy, Erick Otieno, Teddy Kinyanjui, Geoffrey Ndegwa, Jan Vandenabeele, Mary Njenga, and Oliver Johnson. 2014. “Achieving Sustainable Charcoal in Kenya: Harnessing the Opportunities for Cross-Sectoral Integration.” World Agroforestry Center and Stockholm Environment Institute.
International Energy Agency. 2017. World Energy Outlook 2017.
International Energy Agency. 2018. Market Report Series: Energy Efficiency 2018.
Johnson, M., Piedrahita, R., Pillarisetti, A., Shupler, M., Menya, D., Rossanese, M., Delapeña, S., Penumetcha, N., Chartier, R., Puzzolo, E., & Pope, D. (2021). Modeling approaches and performance for estimating personal exposure to household air pollution: A case study in Kenya. Indoor Air, 31.
Lee, K. K., Bing, R., Kiang, J., Bashir, S., Spath, N., Stelzle, D., Mortimer, K., Bularga, A., Doudesis, D., Joshi, S. S., Strachan, F., Gumy, S., Adair-Rohani, H., Attia, E. F., Chung, M. H., Miller, M. R., Newby, D. E., Mills, N. L., McAllister, D. A., & Shah, A. S. V. (2020). Adverse health effects associated with household air pollution: A systematic review, meta-analysis, and burden estimation study. Lancet Global Health, 8 (11).
McCracken, J., Smith, K., Díaz Artiga, A., Mittleman, M., & Schwartz, J. (2007). “Chimney stove intervention to reduce long-term wood smoke exposure lowers blood pressure among guatemalan women. Environmental health perspectives, 115, 996–1001
Pattanayak, S. K., M. Jeuland, J. J. Lewis, F. Usmani, N. Brooks, V. Bhojvaid, A. Kar, L. Lipinski, L. Morrison, O. Patange, N. Ramanathan, I. H. Rehman, R. Thadani, M. Vora, and V. Ramanathan. 2019. “Experimental Evidence on Promotion of Electric and Improved Biomass Cookstoves.” Proceedings of the National Academy of Science of the United States of America 116 (27): 13282–13287.
Pillarisetti, Ajay, Mayur Vaswani, Darby Jack, Kalpana Balakrishnan, Michael N. Bates, Narendra K. Arora, and Kirk R. Smith. 2014. “Patterns of Stove Usage after Introduction of an Advanced Cookstove: The Long-Term Application of Household Sensors.” Environmental Science and Technology 48 (24): 14525–14533.
Republic of Kenya, Ministry of Energy. 2019. “Kenya Cooking Sector Study: Assessment of the Supply and Demand of Cooking Solutions at the Household Level.”
Smith, K., McCracken, J., Weber, M., Hubbard, A., Jenny, A., Thompson, L., Balmes, J., Díaz Artiga, A., Arana, B., & Bruce, N. (2011). Effect of reduction in household air pollution on childhood pneumonia in Guatemala (respire): A randomised controlled trial. Lancet, 378, 1717–26.
Smith-Sivertsen, T., Díaz, E., Pope, D., Lie, R. T., Díaz, A., McCracken, J., Bakke, P., Arana, B., Smith, K. R., & Bruce, N. (2009). Effect of Reducing Indoor Air Pollution on Women’s Respiratory Symptoms and Lung Function: The RESPIRE Randomized Trial, Guatemala. American Journal of Epidemiology, 170 (2), 211–220.
United Nations. 2015. Transforming our World: The 2030 Agenda for Sustainable Development. (A/RES/70/1)
United Nations Human Settlements Programme. (2022). World Cities Report 2022: Envisaging the Future of Cities [ISBN 978-92-1-132894-3].
World Bank 2020b. The State of Access to Modern Energy Cooking Services.
World Health Organization. 2017. The Global Impact of Respiratory Disease.


